Questions
: prepare a 10- to 15-slide Microsoft® PowerPoint® presentation with detailed speaker notes in which you:
- Explain the health disparity or social justice issue related to quality management in today’s health care arena.
- Analyze a problem, system, or process to be improved.
o Address each of the following in your analysis:
? Regulatory, such as OSHA mandate
? Benchmarking
? Improved efficiency
? Patient satisfaction
? Life safety issue
- Analyze a change theory, and incorporate it into your improvement plan.
- Analyze personal leadership theory and style, and incorporate them into your improvement plan.
- Evaluate system changes needed to implement your planned solution, including tools and technologies.
- Create an implementation plan, including a timeline, based on plan-do-study-act (PDSA/PDCA) cycle, including implementation strategies, potential barriers, and evaluation process.
Include at least five peer-reviewed references less than 5 years old(you may not use your course textbooks or Electronic Reserve Reading articles) to support your process improvement and change project
Sample paper
Process Improvement and Change Project
Health disparity or social justice issue related to quality management
- Poor access to healthcare across different socioeconomic, racial and ethnic groups. This is due to:
- Lack of a comprehensive insurance cover.
- Lack of finances.
- Shortage of healthcare providers in rural areas and inner cities.
Poor access to healthcare across different socioeconomic, racial and ethnics groups have been an issue of major concern in the current healthcare arena. Health disparities in the U.S. are common among minority groups such as African Americans, Latinos, Native Americans and the Asia Americans. Poor access to healthcare among these groups is caused by a number of factors. First, majority of people in these minority groups lack a comprehensive insurance cover. For example, migrants who have been in the U.S. for a period less than five years do not qualify for Medicaid. This leads to delays in accessing healthcare. In addition, this group often visits poorly funded clinics which may not fully cater to their needs. Inadequate financial resources has also been a major barrier to accessing quality healthcare. There is shortage of healthcare providers in minority areas such as rural areas and inner cities, compounding the situation further.
Improving the regulatory framework
- Healthcare workers are exposed to numerous work-related hazards.
OSHA can improve safety by developing and enforcing appropriate policies. - OSHA should enforce a safety culture in organizations
- Healthcare organizations should regularly review safety procedures.
- Maintain optimal staff levels and schedules.
Improving the regulatory framework can help in drastically improving patient and healthcare workers safety. Healthcare workers are exposed to a number of health hazards such as drug exposures, biological hazards, blood-borne hazards, radioactive material hazards, and among others (Doyle, Lennox, Bell, 2013). The Occupational Safety & Health Administration (OSHA) is mandated to provide a safe environment to both the patients and healthcare workers. OSHA can improve safety in healthcare organizations by developing and enforcing appropriate policies. For instance, OSHA should enforce a safety culture in all healthcare organizations. Healthcare organizations should regularly review safety procedures and train healthcare workers on the same. Staff levels and schedules should be kept optimal to avoid long shifts which exhausts the healthcare workers.
Benchmarking
- Benchmarking can significantly help in improving healthcare organizations’ systems and processes.
- Benchmarking involves voluntary collaboration which improves quality.
- Statistical methods should be employed in benchmarking.
- Healthcare organizations should extend benchmarking to other sectors such as financial management practices.
According to Ettorchi-Tardy, Levif & Michel, (2012), benchmarking in healthcare refers to collaboration among healthcare organizations in order to compare processes and improve organizational performance. Benchmarking can significantly help in improving healthcare organizations’ systems and processes. Not only does benchmarking involve the use of comparison indicators but also foster voluntary collaboration between healthcare organizations for the purpose of improving quality. Statistical methods should be employed during the process of benchmarking to improve the process. Areas of clinical performance to be measures or compared should be keenly identified. This may involve the quality, structure and clinical outcomes. Healthcare organizations should extend benchmarking to other sectors too such as in financial management practices, rather than dwelling on improving quality of care.
Improved efficiency
- Improved efficiency calls for reduced wastage and careful allocation of resources.
- Emergency department should only be used for crucial cases.
- Improving the discharge process.
- Physicians to maintain professionalism.
Currently, healthcare organizations are focusing on day-to-day quality improvement so as to enhance efficiency in service delivery. Healthcare organizations are looking for ways to tackle issues to do with quality of services delivered, safety of procedures, and equality in access to healthcare. In order to improve efficiency, healthcare organizations must reduce waste and allocate resources in a sustainable way. There are a number of strategies that healthcare organizations can use to improve efficiency. First, healthcare organizations should ensure that the emergency department is only used for necessary cases. Second, the discharge process should be improved to avoid keeping inpatients for unnecessarily lengthy periods. Physicians should focus more on maintaining professionalism by acting on the best interest of the patients. Lastly, federal and local governments should provide more material and technical support to healthcare organizations to enable them deliver quality care.
Patient satisfaction
- Patient satisfaction is related to quality of care.
- Patient satisfaction can be improved by better provider communication skills.
- Maintaining professionalism.
Patient satisfaction in healthcare organizations is directly related to the quality of care provided. Feedback from patients is used to gauge satisfaction levels. Simple strategies can improve patient satisfaction in healthcare organizations. Patient satisfaction can be enhanced by improving provider communication skills. According to Selby, Beal, and Frank (2012), improved communication leads to patient adherence to prescription, reduced risk of malpractice, better understanding of the patient problem and favorable clinical outcomes. It is also important for physicians to maintain professional ethics in their work. Some physicians may dwell more on the economic gains rather than on the well-being of the patient. High patient satisfaction can also be achieved by improving the quality of care accorded to patients.
Life safety issues
- Hallways should be unobstructed
- Broken door seals should be regularly fixed.
- Proper fire rating on doors.
There are a number of life safety issues in healthcare organizations. Generally, healthcare organizations should aim at improving life safety issues so as to avoid unnecessary injuries and deaths. Healthcare organizations should ensure that hallways are not obstructed. This ensures there is easy access to exit doors as well as the stairwells. Broken door seals should be regularly fixed. These may cause hazards such as fire to spread quickly. The hospital should also provide proper fire rating on doors (Al-Abri & Al-Balushi, 2014).
Change theory
- Lewin’s Change Management Theory can support changes in the organization.
- The first stage involves creating an atmosphere for change.
- The second stage involves analyzing the type of changes to be made and the mechanisms for change.
- The last stage involves integrating the new changes into the organization.
Lewin’s Change Management Theory can be an appropriate change management theory in a healthcare setting. The theory supports changes in organizations by enhancing a smooth transition. Lewin’s theory takes a three-stage approach to change. The three stages include unfreezing, moving, and lastly refreezing (Liu, Akram, & Bouguettaya, 2011). In the unfreeze stage, an atmosphere for change is created in the organization. The second stage involves analyzing the changes to be made and the type of mechanisms to be used. The last stage involves integrating the new changes and ensuring operations flow as prior to the implemented changes. Lewin’s Change Management Theory can be incorporated when changing the medical administration method from manual order entries to the use of bar-coding.
Personal leadership theory and style
- Behavioral foundations theory which is based on personality.
- Democratic leadership is the best suited style of leadership.
- Democratic leaders engage employees in decision making.
My personal leadership theory is hinged on the premise of behavioral foundations. The behavioral theory of leadership asserts that the personality of an individual determines his/her leadership effectiveness. As such, important characteristics such as self-confidence and a positive ego can go a long way in developing leaders. The best style of leadership is democratic leadership. Democratic leaders engage employees in the decision making process. This makes employees feel valued. In addition, employees work hard to solve any problems since they actively contribute the decision making process by giving possible solutions. In order to incorporate the leadership theory into the improvement plan, there is need to hold regular meetings where physicians can brainstorm on possible solutions to problems.
System changes for the planned solution
- Propose a bar-coding medication administration system.
- Automated pharmacy dispensing system.
There are a number of system changes that should be carried out in order to enhance efficiency and delivery of quality services at the healthcare organization. There should be a bar-coding medication administration system in place in order to reduce medical errors. This should also include automated pharmacy dispensing system at the healthcare organization. Scanning and bar-coding of medications is a revolutionary technology that can help reducing medication errors (Hardmeier, A., et al., 2014). It can also improve service delivery. Implementation of this technology will require coded medication covers, patient identification bands and medication carts. In using this system, nurses will be scanning the patients’ identification bands with the scanner and information obtain compared with that in the hospital’s medication administration record database.
Implementation plan, including a timeline
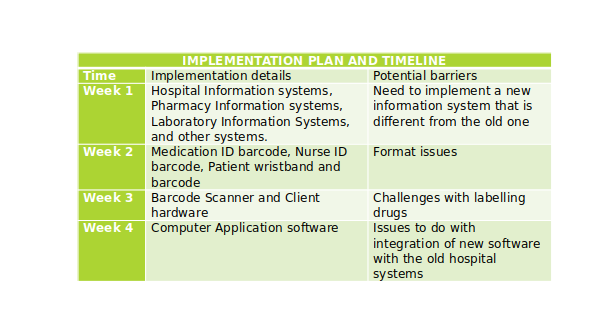
Implementation will involve a careful study of the existing hospital system in order to avoid issues. During the implementation phase, a committee should be formed comprising of members from various departments to be affected such as administration, nursing, laboratory, pharmacy and IT. The evaluation process will entail thorough review and testing of the new system to ensure it delivers as expected.
References
Al-Abri, R., & Al-Balushi, A. (2014). Patient Satisfaction Survey as a Tool Towards Quality Improvement. Oman Medical Journal, 29(1), 3–7. http://doi.org/10.5001/omj.2014.02
Doyle C, Lennox L, Bell D. A (2013). systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open. 2013;3(1):e001570.
Ettorchi-Tardy, A., Levif, M., & Michel, P. (2012). Benchmarking: A Method for Continuous Quality Improvement in Health. Healthcare Policy, 7(4), e101–e119.
Hardmeier, A., et al. (2014). Pediatric Medication Administration Errors and Workflow following Implementation of Bar Code Medication Administration System. Journal of Healthcare Quality, 36(4): 1-36.
Liu, X., Akram, S., & Bouguettaya, A. (2011). Change management for semantic web services. New York: Springer.
Selby, J., Beal, A. C., Frank, L. (2012). The Patient-Centered Outcomes Research Institute (PCORI) National Priorities for Research and Initial Research Agenda. JAMA : The journal of the American Medical Association, 307(15):1583-1584.
Veterans Administration Medical Center-Structure and Culture